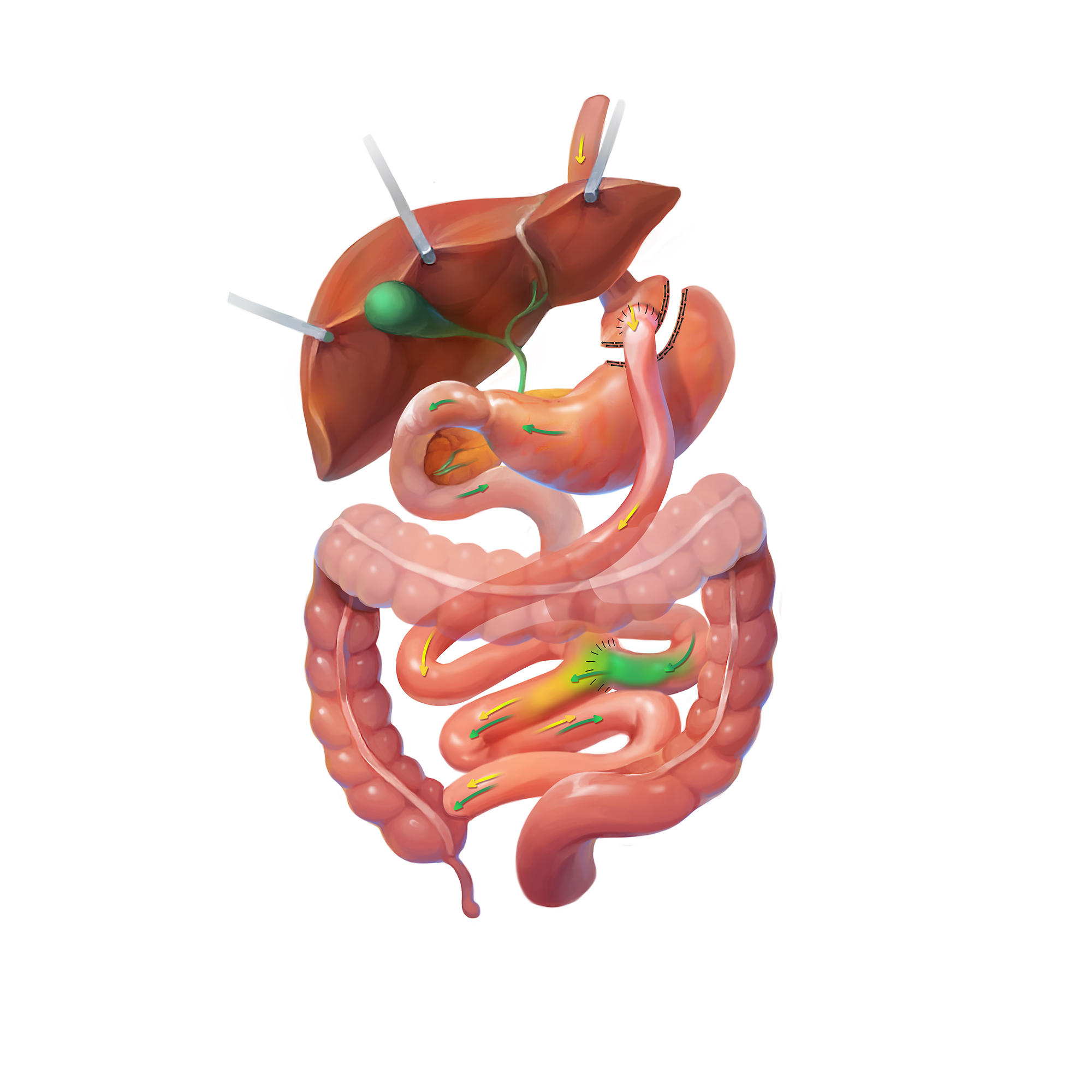
The gastric bypass was first performed many decades ago and quickly became the gold standard in bariatric surgery. This was due to the excellent safety profile, combined with very good long-term weight loss and disease improvement results. The gastric bypass, while not the most popular bariatric surgical procedure anymore, does offer exceptional benefits to many patients, especially those who suffer from uncontrolled diabetes or acid reflux.